ADVERTISEMENT
Filtered By: Lifestyle
Lifestyle
Preventing cervical cancer among teens, and at any age
By ALICE M. SUN-CUA
Women Talk
Sarah, a 42-year-old businesswoman, came to see me because of vaginal bleeding after sexual intercourse. She was single and had never been pregnant, so she thought she didn’t need to see a gynecologist, especially because she was very busy with work.
 Upon examination, a two-centimeter cervical growth was noted. It bled easily. I did a biopsy at the clinic and the final verdict was cervical cancer, in its early stage. This meant there was no involvement of any area in the upper vagina, nor the region where the fallopian tubes and ovaries are located.
Upon examination, a two-centimeter cervical growth was noted. It bled easily. I did a biopsy at the clinic and the final verdict was cervical cancer, in its early stage. This meant there was no involvement of any area in the upper vagina, nor the region where the fallopian tubes and ovaries are located.
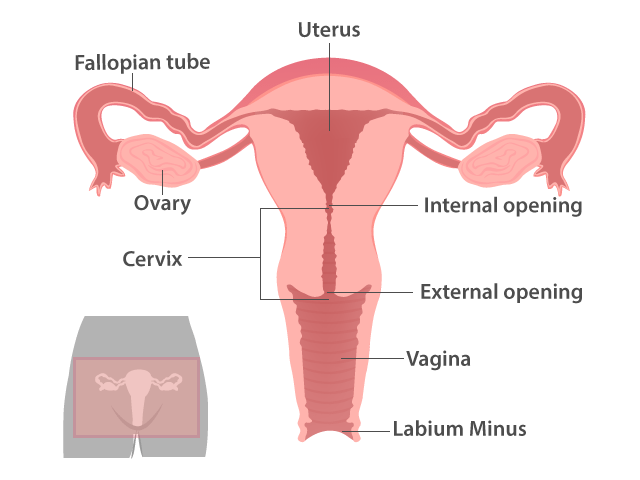
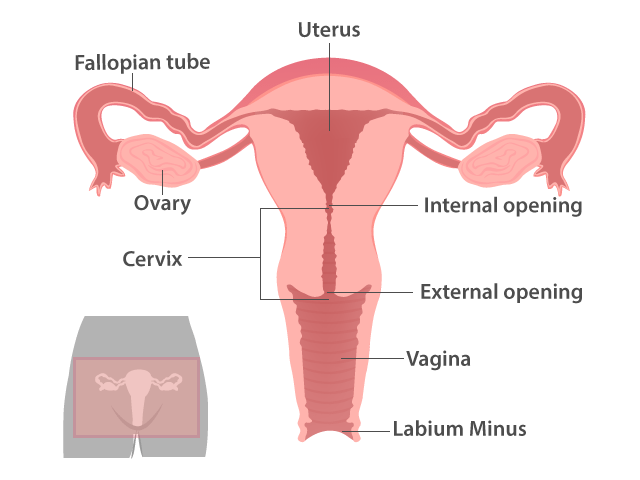
But where is the cervix? Is it related to the uterus? This simple anatomical diagram of the female pelvic organs would answer these questions.
Teenage sex and multiple partners
The cause of cervical malignancy, like any cancer, used to be unknown. But in recent years, scientists have isolated several human papilloma viruses (HPV) that have been strongly linked to cervical cancer.
Evidence has now associated cervical cancer with sexual activity at a young age. For teenage girls, it has been hypothesized that because the transitional layer of the cervix is still exposed, it is easily affected by any harmful factor as the zone is susceptible to developing malignant tumors.
Being exposed to multiple partners also increases the chances of having the disease. It helps to remember that because a woman could not get the HPV infection alone, it pays to be monogamous, and the male partners to be monogamous as well.
Thus, prevention is still the best strategy.
Pap’s Smear
An annual Pap’s Smear is strongly advised for women who are 35 years of age—regardless of or even with no sexual activity, as there have been cases of virginal women developing cervical cancer—and for any girl who is already active sexually, regardless of age.
Because of the many stories heard from friends, however, women’s usual reaction to Pap’s Smear is fear and avoidance. It is supposed to be a long, painful process with the woman lying on the examining table, legs spread out. Such an inelegant position, one of my patients commented.
The truth is that the actual process takes less than one minute. What takes long is the mental preparation of the patient – removing her undergarments, ascending the examining table, and positioning her legs over the stirrups that are about two feet apart. There is a lamp focused on her vulva. The doctor is seated before her splayed legs, and the patient is asked to relax, and not close or clamp her leg muscles. This preparation alone, especially for first timers, takes time.
Do find a doctor who is patient enough to explain what to expect, someone you are comfortable with, even if it is the first time that you’ve met.
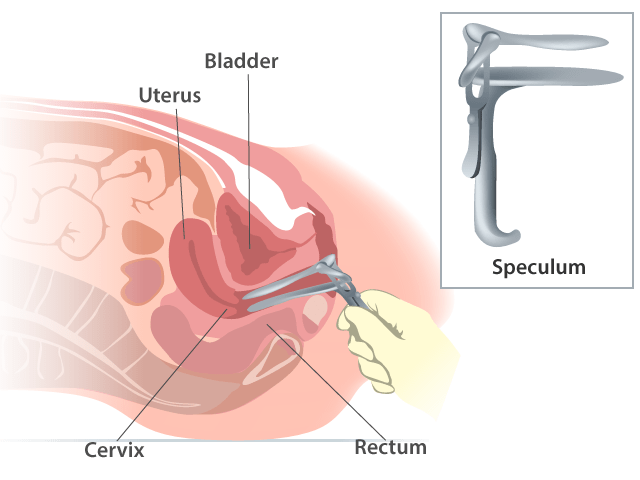 The doctor will gently insert an instrument called a speculum into your vagina; there are many sizes for speculums, and I usually use a smaller and slimmer one for women who are single and not active sexually.
The doctor will gently insert an instrument called a speculum into your vagina; there are many sizes for speculums, and I usually use a smaller and slimmer one for women who are single and not active sexually.
The speculum will feel a little cold (it is made of steel) and the doctor will open it slowly to look at the cervix. She will note any unusual growths, or discoloration. Some doctors will swab the cervix with acetic acid to note any “white areas” (where the acid was not absorbed) and thus “suspicious,” and may do a biopsy of these areas.
The doctor will also see if there are abnormal discharges that could mean infection. If there are gross signs of infection, treatment will first be given before a Pap’s Smear is done. This is because infection will obscure any good cellular inspection for malignancy.
Then the doctor will do a smear: with a wooden spatula or a small brush, she will take a sample by gently scraping the area around the cervical opening. After this she will spread the smear on a clean glass slide (or, in the case of the brush, put the end of the brush on a solution in a small vial). The glass slide is fixed with hair-spray—that is why you sometimes find a bottle of hair-spray in your gynecologist’s clinic—or formaldehyde. These are all sent to the pathologist, who will check the slide under the microscope to look for abnormal cells that might signal malignancy.
After the Pap’s Smear, a pelvic exam is routinely done. This involves bimanual palpation, which means that the doctor's two gloved fingers will be inside the vagina and her other hand outside on your abdomen, pressing gently, checking for any enlargement of the uterus, fallopian tubes, or ovaries. In this manner, the Pap’s Smear schedule is also an opportunity for a thorough gynecologic exam.
Are HPV vaccines advisable?
Lately, there has been a surge in high-profile advertisements of vaccines to prevent cervical cancer. These are breakthroughs, indeed, as cervical cancer is still high in our statistics as a cause of mortality in Philippine women.
These vaccines essentially provide protection against infections from HPV. One of them is against two viruses, and the other, against four. These HPV viruses are the most common causes of cervical cancer, but there are still other HPV viruses that could cause the malignancy. It is also important to note that viruses are not the only cause of cervical cancer; other non-infectious risk factors include a positive family history, smoking, poor nutrition, and a low immune defense system.
The vaccines are given on three scheduled visits over a period of six months. The best population for these vaccines are girls 9 to 16 years old, especially those that are not yet sexually active. Older women until the age of 45, the maximum age of the clinical trials, could also be given vaccines.
Bleeding and other symptoms
There are no definite signs and symptoms for early cervical cancer. It is a slow-growing malignancy, but when vaginal bleeding occurs, there is usually a mass already that can be seen through a gynecological exam.
If found early, surgery is done. If the disease is already advanced and surgery is no longer helpful, chemo or radiotherapy may be given.
As for Sarah, I referred her to a gynecologic oncologist, who scheduled her for surgery. The prognosis was good, as the malignancy was detected early. – With illustrations by Analyn Perez/YA, GMA News
Sarah, a 42-year-old businesswoman, came to see me because of vaginal bleeding after sexual intercourse. She was single and had never been pregnant, so she thought she didn’t need to see a gynecologist, especially because she was very busy with work.
 Upon examination, a two-centimeter cervical growth was noted. It bled easily. I did a biopsy at the clinic and the final verdict was cervical cancer, in its early stage. This meant there was no involvement of any area in the upper vagina, nor the region where the fallopian tubes and ovaries are located.
Upon examination, a two-centimeter cervical growth was noted. It bled easily. I did a biopsy at the clinic and the final verdict was cervical cancer, in its early stage. This meant there was no involvement of any area in the upper vagina, nor the region where the fallopian tubes and ovaries are located.But where is the cervix? Is it related to the uterus? This simple anatomical diagram of the female pelvic organs would answer these questions.
Teenage sex and multiple partners
The cause of cervical malignancy, like any cancer, used to be unknown. But in recent years, scientists have isolated several human papilloma viruses (HPV) that have been strongly linked to cervical cancer.
Evidence has now associated cervical cancer with sexual activity at a young age. For teenage girls, it has been hypothesized that because the transitional layer of the cervix is still exposed, it is easily affected by any harmful factor as the zone is susceptible to developing malignant tumors.
Being exposed to multiple partners also increases the chances of having the disease. It helps to remember that because a woman could not get the HPV infection alone, it pays to be monogamous, and the male partners to be monogamous as well.
Thus, prevention is still the best strategy.
Pap’s Smear
An annual Pap’s Smear is strongly advised for women who are 35 years of age—regardless of or even with no sexual activity, as there have been cases of virginal women developing cervical cancer—and for any girl who is already active sexually, regardless of age.
Because of the many stories heard from friends, however, women’s usual reaction to Pap’s Smear is fear and avoidance. It is supposed to be a long, painful process with the woman lying on the examining table, legs spread out. Such an inelegant position, one of my patients commented.
The truth is that the actual process takes less than one minute. What takes long is the mental preparation of the patient – removing her undergarments, ascending the examining table, and positioning her legs over the stirrups that are about two feet apart. There is a lamp focused on her vulva. The doctor is seated before her splayed legs, and the patient is asked to relax, and not close or clamp her leg muscles. This preparation alone, especially for first timers, takes time.
Do find a doctor who is patient enough to explain what to expect, someone you are comfortable with, even if it is the first time that you’ve met.
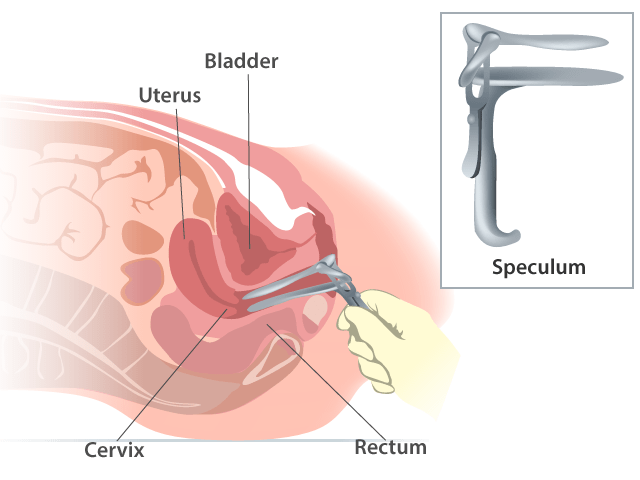 The doctor will gently insert an instrument called a speculum into your vagina; there are many sizes for speculums, and I usually use a smaller and slimmer one for women who are single and not active sexually.
The doctor will gently insert an instrument called a speculum into your vagina; there are many sizes for speculums, and I usually use a smaller and slimmer one for women who are single and not active sexually.The speculum will feel a little cold (it is made of steel) and the doctor will open it slowly to look at the cervix. She will note any unusual growths, or discoloration. Some doctors will swab the cervix with acetic acid to note any “white areas” (where the acid was not absorbed) and thus “suspicious,” and may do a biopsy of these areas.
The doctor will also see if there are abnormal discharges that could mean infection. If there are gross signs of infection, treatment will first be given before a Pap’s Smear is done. This is because infection will obscure any good cellular inspection for malignancy.
Then the doctor will do a smear: with a wooden spatula or a small brush, she will take a sample by gently scraping the area around the cervical opening. After this she will spread the smear on a clean glass slide (or, in the case of the brush, put the end of the brush on a solution in a small vial). The glass slide is fixed with hair-spray—that is why you sometimes find a bottle of hair-spray in your gynecologist’s clinic—or formaldehyde. These are all sent to the pathologist, who will check the slide under the microscope to look for abnormal cells that might signal malignancy.
After the Pap’s Smear, a pelvic exam is routinely done. This involves bimanual palpation, which means that the doctor's two gloved fingers will be inside the vagina and her other hand outside on your abdomen, pressing gently, checking for any enlargement of the uterus, fallopian tubes, or ovaries. In this manner, the Pap’s Smear schedule is also an opportunity for a thorough gynecologic exam.
Are HPV vaccines advisable?
Lately, there has been a surge in high-profile advertisements of vaccines to prevent cervical cancer. These are breakthroughs, indeed, as cervical cancer is still high in our statistics as a cause of mortality in Philippine women.
These vaccines essentially provide protection against infections from HPV. One of them is against two viruses, and the other, against four. These HPV viruses are the most common causes of cervical cancer, but there are still other HPV viruses that could cause the malignancy. It is also important to note that viruses are not the only cause of cervical cancer; other non-infectious risk factors include a positive family history, smoking, poor nutrition, and a low immune defense system.
The vaccines are given on three scheduled visits over a period of six months. The best population for these vaccines are girls 9 to 16 years old, especially those that are not yet sexually active. Older women until the age of 45, the maximum age of the clinical trials, could also be given vaccines.
Bleeding and other symptoms
There are no definite signs and symptoms for early cervical cancer. It is a slow-growing malignancy, but when vaginal bleeding occurs, there is usually a mass already that can be seen through a gynecological exam.
If found early, surgery is done. If the disease is already advanced and surgery is no longer helpful, chemo or radiotherapy may be given.
As for Sarah, I referred her to a gynecologic oncologist, who scheduled her for surgery. The prognosis was good, as the malignancy was detected early. – With illustrations by Analyn Perez/YA, GMA News
Dr. Alice M. Sun-Cua is an author and practicing obstetrician-gynecologist at the San Juan de Dios Hospital in Pasay City.
More Videos
Most Popular




