ADVERTISEMENT
Filtered By: Lifestyle
Lifestyle
Women Talk: When heavy bleeding occurs around menopause
M., a 47-year-old hotel employee, came to see me one year ago because of heavy menstrual bleeding for almost a month. A pelvic ultrasound showed that the inner lining of her uterus (endometrium) was still thick even after the bleeding; normally, the endometrium thins out after the menses.
Abnormal hormonal levels during the years approaching menopause could cause such bleeding. This means the normal hormones of the body are no longer secreted in a cyclical and timely manner, and in amounts sufficient enough to produce an orderly interval, amount, and duration of the monthly menstrual bleeding.
Perimenopause (or “around the menopause”) is that time when the ovaries, because of age, no longer secrete enough hormones to keep the menses regular. This triggers a feedback to the brain, causing it to “whip” the ovaries to produce the usual amounts. However, because of ovarian aging (nature’s way of telling us that the body has reached its limit for reproduction), the ovaries will fail to respond to this stimulation.
At times, doctors will request for the level of the follicular-stimulating hormone in women 40 and above to check if it is increased: if it is, then it is presumed that the woman is already in her perimenopause.
Many women in their late 40s simply stop menstruating. If a woman's cycles are absent for at least 12 months, we can say that she is already in menopause. However, most women start having skipped menses at around this time, with the amount getting scantier and the intervals longer.
When menses do not come on time, of course the first thing that comes to mind is pregnancy, especially when the woman is sexually active. When that is ruled out (there’s a more sensitive blood exam for this now), I usually advise my patients to keep a “menstrual diary” where she marks the days of bleeding, including the amount. We expect that after these irregular days, the menses will finally stop.
Polyps
Some women, however, will have a difficult transition. Menses become heavy, prolonged, and accompanied by abdominal pain. Many have to use diapers during their periods. In many cases the bleeding becomes so profuse that the woman becomes weak, pale, and anemic. A few will even need blood transfusion if the blood levels become very low.
A lot of women hope that the bleeding will spontaneously stop, so they will wait for some time before consulting the doctor.
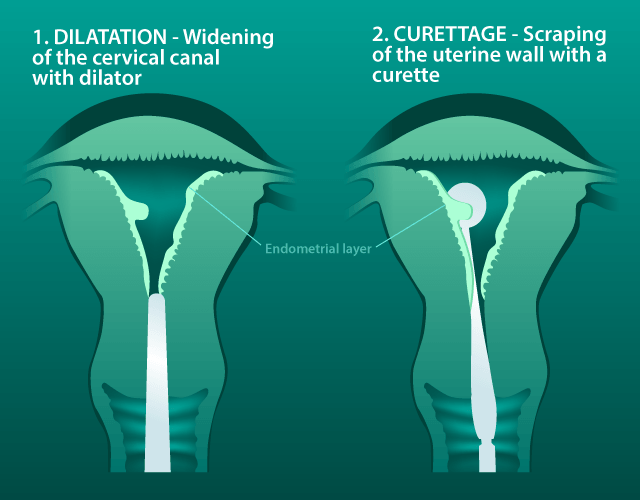
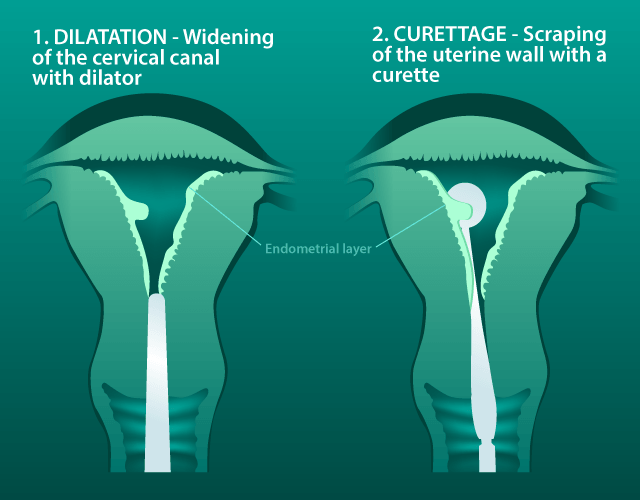
To stop the bleeding, curettage will need to be done. This means that under anesthesia (usually regional like epidural or spinal) the uterus is “cleaned out” using a curette.
Contrary to popular belief, curettage does not “thin out” the uterus. A D&C (dilatation and curettage) will scrape out only the upper functional layer of the endometrium, and will leave the basal layer intact. This functional layer is the one that is removed or sloughed off during the monthly menses, leaving the basal layer to regenerate. After the endometrial layer lies the muscular, thick layer of the uterus, making up most of its bulk, and finally the “wrapper,” the serosal layer. There is no truth then to the idea that curettage will make the uterus “thinner.”
The tissues obtained from this procedure are sent to the pathologist for microscopic evaluation. The doctor will usually prescribe an iron and vitamin tablet to the woman as a supportive measure.
Contrary to popular belief, curettage does not “thin out” the uterus. A D&C (dilatation and curettage) will scrape out only the upper functional layer of the endometrium, and will leave the basal layer intact. This functional layer is the one that is removed or sloughed off during the monthly menses, leaving the basal layer to regenerate. After the endometrial layer lies the muscular, thick layer of the uterus, making up most of its bulk, and finally the “wrapper,” the serosal layer. There is no truth then to the idea that curettage will make the uterus “thinner.”
The tissues obtained from this procedure are sent to the pathologist for microscopic evaluation. The doctor will usually prescribe an iron and vitamin tablet to the woman as a supportive measure.
At times the pathology report will show an “endometrial polyp” (as in the case of my patient M.) which is a benign growth of the lining. No further medications are given to these patients.
High estrogen
In some, “simple” or “complex” hyperplasia is reported by the pathologist. This means that there is a high level of estrogen in the body, in spite of the failing ovaries.
So what are the other sources of estrogen, then?
Above our kidneys are small organs called the suprarenal glands, and they are sources of extra-ovarian estrogen.
In the body too, are hormones that could be converted to estrogen during the menopause. This conversion happens in the adipose (fat) tissues, so logically, the more fat one has, the more conversion there will be. More estrogen in circulation causes more thickening of the endometrial lining, leading to profuse bleeding.
Incidentally, it is also because of this fat layer that overweight women in their perimenopause seldom have problems with hot flushes.
Endometrial cancer
The bad news, of course, is that perimenopausal bleeding, and thickening of the lining, could also mean endometrial cancer. That is why doctors insist on a pathologic diagnosis before doing anything, even reassurance.
Endometrial cancer arises from too much estrogen in the body, and its symptom is similar to those of endometrial polyps and hyperplasia: vaginal bleeding. Therefore the curettage, done to stop the profuse bleeding, is also diagnostic in nature because the samples are sent to the laboratory for the final diagnosis.
During perimenopause, some women on pelvic ultrasound show “thick endometrial lining” but have no symptoms. We can usually do an endometrial biopsy in the clinic, mainly to have a tissue diagnosis, and to allay our fears of a malignancy.
My patient M. came back to me after one year because of the same problem: profuse bleeding. She had been well for more than a year, she said, with regular menses. Again, a thick endometrial lining was seen in a pelvic ultrasound, and she underwent another curettage.
This time, the findings in M’s scrapings showed “simple hyperplasia,” which means that she has high levels of estrogen, and that there is a danger it could progress to malignancy.
Hyperplasia itself is not cancer, but some doctors would advise the removal of the uterus and the ovaries for women in perimenopause because of the fear of its progression.
Other doctors would start these women on progesterones, and many patients respond by having regular menses, until they reach menopause.
Do not wait too long for a consultation when bleeding occurs during perimenopause. A lot can be done, and the earlier you see your doctor, the better. —With illustration by Analyn Perez/YA, GMA News
Tags: womentalk, womenshealth
More Videos
Most Popular




